Human hormonal system
We are made up of several tens of trillions of cells grouped into organs and tissues. And in order to survive, each of these cells must not only work in a well-coordinated team with the others, but also strictly obey orders from above on the central nervous system (consisting, again, of neuron cells). Only such strict subordination and effective interaction transform a huge aggregate of cells into a highly organized competitive biological machine, where cells have different specializations, but all work to achieve one simple goal - the survival of the whole team (the whole organism).
Hormones are a way for some cells to communicate and control others. Hormones are signaling molecules that are used to communicate between different organs and tissues to regulate physiological and behavioral processes, such as: digestion, metabolism (metabolism), respiration, sleep, stress, growth and development of the body, reproduction, mood, sleep cycle - waking, work of the immune system, feeling of hunger, preparing the body for mating, fighting, running away, preparing the body for a new phase of life (puberty, menopause), excretion, lactation and so on. The word "hormone" is translated from Greek as "excite, impel." It will be much easier for you to understand the role of hormones, if in your mind you replace them with the word "signalmen" every time: a signalman, cortisol, a signalman, testosterone, a signalman, T3, and so on.
Hormones are produced by various glands and transported to the circulatory system. In order for a hormone to transmit a signal to a cell, it must first communicate with the corresponding cell receptor, which should not be resistant. It is all the same to the body how much hormones are walking through your bloodstream, only the amount that effectively binds to the receptor is important. Therefore, even if you have a completely healthy concentration of thyroid hormones in the bloodstream, but with pathologically low cortisol / zinc / iron (the receptors will be resistant), you will receive hypothyroidism, which will not be eliminated by taking additional hormones. In fact, they will worsen your condition rather than improve. This important difference between the bloodstream and the cell, alas, most doctors do not understand. If they see that the concentration of free T3 and free T4 in the bloodstream is “healthy”, then they automatically assume that there is no hypothyroidism, even if the TSH clearly calls for help (more than 2).
All hormones circulate in the bloodstream in two forms - free and bound. Since the half-life of various hormones in a free form is very short (20-30 minutes in some, 100 minutes in cortisol), most of the hormones (in some under 90%) are associated with proteins: globulins and albumin. The linked form is essentially a long-term storage method for hormone stocks. Only free form is biologically active. Therefore, it is on her and need to be tested. Unfortunately, 99% of endocrinologists in Russia, when assessing cortisol levels, are sent to total cortisol in the blood instead of free in daily urine or saliva, which is an unforgivable mistake and very often confuses the doctor and the patient. In most cases of adrenal insufficiency, total cortisol in the blood is just the same, and only a test for free cortisol allows you to diagnose the problem.
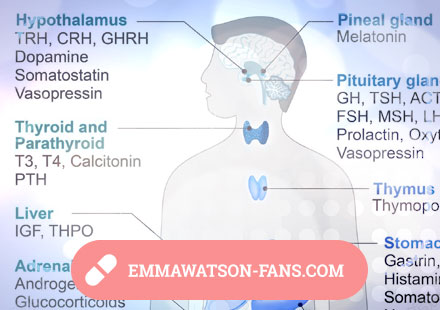
The human hormonal system is divided into glandular (where endocrine cells are gathered together and form the endocrine glands or "glands" in English) and diffuse, where endocrine cells are scattered throughout the body. The glandular endocrine system is controlled by the hypothalamus and pituitary. A hypothalamus is a small area of the brain that actually communicates between the nervous system (brain) and the endocrine system (endocrine glands) through the pituitary gland (orchestra conductor). The hypothalamus is actually the "CEO" of the endocrine system, which gives orders to its first deputy, the pituitary gland, and that, in turn, already controls the other glands, such as the thyroid, adrenal glands, pancreas, sex glands, etc.
The pituitary gland communicates with various glands with the help of tropic hormones. For example, thyroid-stimulating hormone stimulates the thyroid gland to secrete its hormones into the blood, adrenocorticotropic hormone (ACTH) stimulates the adrenal glands, gonadotropins stimulate the sex glands to produce sex hormones, and so on. That is, when the pituitary gland increases the production of thyroid-stimulating hormone - it actually signals the thyroid gland to "produce more hormones!". When significantly reduces - it signals "produce less." The function of tropic hormones is to signal various glands, in what volume they need to produce and secrete their own hormones into the blood. Try to read this paragraph again, replacing the word "hormone" in your mind with the word "signalman", so it will be much easier to remember.
The hypothalamus communicates with the pituitary gland using so-called "liberins" (or releasing hormones, or releasing factors), which stimulate the secretion of various tropic hormones of the pituitary, as well as statins - which inhibit the secretion of tropic hormones. For example, the hypothalamus signals the pituitary gland, secreting thyroliberin (or tyroetropin-releasing hormone), and in response, the pituitary gland signals the thyroid gland, secreting the thyretropic hormone. Such a scheme of work forms various hypothalamic-pituitary arches: hypothalamus-pituitary-thyroid, hypothalamus-pituitary-adrenal glands, hypothalamus-pituitary-ovaries, and so on.
The glandular endocrine system is represented by the following glands: thyroid, pancreas, adrenal glands, parathyroid glands, pineal gland (also known as pineal gland), gonads (sex glands: ovaries in women and testicles in men), thymus.
Diffuse system. Some endocrine functions are performed by the liver (secretion of somatomedin, insulin-like growth factors, etc.), kidney (secretion of erythropoietin, medullins, etc.), stomach (secretion of gastrin), intestines, spleen (secretion of splenitis), etc. Endocrine cells are contained throughout the body person
Symptoms of hypothyroidism
Since the thyroid hormones regulate the rate of energy supply to the body cells, with hypothyroidism all processes slow down, the functionality of all organs and systems, including the brain, decreases.
All the symptoms I would break into two groups: 1) manifested in the majority and 2) manifested only in some patients
The main symptoms of hypothyroidism, which manifest themselves in the absolute majority of patients:
1) Chronic fatigue, fatigue, weakness.
2) Hypothermia (low body temperature). Measured under the tongue and well reflects the metabolic rate. Rarely, in hypothyroidism, it can be high due to low iron stores, low aldosterone, low estradiol, and excess adrenaline.
3) Endogenous depression. If you ask hypothyroids if they have endogenous depression, then 90% will mistakenly say that "NO." As practice shows, the absolute majority of people misunderstand this term. They see depression as a feeling of intense heartache, irresistible anguish, anxiety, guilt feelings, and a depressed person is a person who does not want anything, voluntarily isolates himself from society, expresses pessimistic thoughts, often cries, looks at one point, and so on. In fact, this term is much broader, and it means the internal state of the brain in which you lose the taste for life, the level of pleasure from it drops significantly, everything seems more uninteresting and boring than it actually is. You are more difficult to laugh or to please. If the brain of a healthy person responds to positive events with joy and elevation of mood, tentatively speaking, by 10 points, then for a person with endogenous depression - only 3-5. This term does not mean that your interest in life has dropped to zero and you are thinking about suicide, or that you never laugh at all, do not rejoice in anything and are in sorrow. It just means that your brain reacts to positive events with significantly lower levels of joy, pleasure and mood elevation than it does in healthy people. The degree of manifestation of endogenous depression also depends on the worldview, character, positive / negative thinking and a number of other factors. Doctors divide all depressions into reactive (as a reaction to objectively existing external adverse events such as the loss of a loved one, work, etc.) and endogenous (that is, internal), when the cause of depression is a violation of the metabolism of neurotransmitters (serotonin, dopamine, GABA and others) and little depends on external circumstances. Since thyroid hormones, cortisol, insulin, testosterone, and estradiol are involved in regulating the metabolism of neurotransmitters, a drop in any of these hormones will lead to endogenous depression. Exactly like diabetes. Running through psychotherapists in such situations is a hopeless undertaking, since the only thing they can do is temporarily alleviate the symptoms of taking antidepressants, a long (9 months) reception of which in the studies aggravates depression even more than before they began.
4) Brain fog, poor short-term memory, forgetfulness. Difficulties with long-term concentration. Your brain thinks more slowly than before. Brain fog can subjectively not be felt if you do not load the brain with voluminous tasks with a time limit.
5) Poor exercise tolerance.
6) Active hair loss + brittle nails + dry skin. Thinning of the outer edges of the eyebrows. Very often, hypothyroidism wear short hairstyles due to the fact that the hair becomes dry, weak and brittle and they have to cut their hair short.
7) Often freezing feet. Sensitivity to cold. An absolutely normal situation for a hypothyroid is to sit in two pairs of socks. Personally, I never had the sensation of cold, but my feet were always cold. And I, of course, wrote it off as a feature of my body, until I tried to take T3 and my feet became warmer.
8) Weakened immunity. You become more vulnerable to various kinds of infections, and recovery takes longer than usual.
9) Weakened libido.
The following symptoms may occur in some people and not in others:
1) Easy set of fat mass and serious difficulties from its disposal. This symptom is often present in women and less often in men. Since the slower energy metabolism consumes less, all the unspent energy the body sends to the stock. Thus, the hypothyroidism can eat absolutely adequately, without overeating, but at the same time regularly gaining weight, since the calories supplied from food are not consumed at the proper speed due to T3 deficiency at the cellular level. Accordingly, it will be hard to lose weight in such a situation, although it is possible. Of course, whether fatty hypothyroidism will gain weight depends on other factors, such as genetic predisposition, testosterone / estradiol balance, leptin resistance, the amount of fast carbohydrates in the diet, the total amount of carbohydrates, the presence or absence of physical exertion, etc. In practice, most women gain weight. Among men, a different situation - some are gaining fat, others are not. Personally, I never became fat even with deep hypothyroidism and cortisol deficiency. The only periods when I gained fat were when I rocked in the hall and purposefully ate a lot over appetite. Both muscle and fat mass grew - which is quite predictable. I also saw a lot of guys with hypothyroidism with low body fat%.
2) Excessive and non-refreshing sleep for 9-10 hours. Difficulty falling asleep and / or frequent waking up.
3) Problems with pulse and pressure.
4) Chronic irritability. Increased anxiety. Bipolar disorder. Anger. Paranoia.
5) Allergies (can also be a symptom of low cortisol)
6) Irritability. Anxiety Panic attacks. They are less common and more often the result of low cortisol.
7) Digestive problems. Constipation. Bloating. Heartburn. Small pimples on the forehead (problems in the small intestine).
8) Irregular menstrual cycle or lack thereof. Abundant periods.
9) Puffiness \ swollen face.
10) Pain when swallowing. Appears only in a small number of patients during goiter development.
11) Enhanced appetite or vice versa weakened appetite.
12) Insulin resistance. T3 deficiency or T3 excess - both in studies lead to insulin resistance, i.e. to the degree of pre-diabetes or diabetes.
13) Hoarseness
14) Muscle cramps
15) Reactivation of Epstein-Barr virus.
16) Regularly recurrent candidiasis (thrush). Candida loves low temperatures and it is extremely difficult to get rid of it with hypothyroidism. First, cure hypothyroidism, then remove candidiasis.
Since hypothyroidism in many people leads to a drop in adrenal function (hypocorticism), it is also worthwhile to evaluate the symptoms of low cortisol and aldosterone.
Temperature monitoring
Sublingual temperature and symptoms are the best indicators of metabolic rate, so it is by monitoring temperature (and not TSH) that the effectiveness of treatment and dosage of hormone replacement therapy can be monitored. Unfortunately, the absolute majority of doctors treats and selects the dose exactly as they were taught several decades ago: every 2-3 months they direct the patient to retake the TSH, trying to find the T4 dose that would drive the TSH to the unit. Such a strategy is an unforgivable mistake and leaves most patients with untreated hypothyroidism. According to reviews of a huge number of hypothyroids, an effective dose of natural dried thyroid glands gives them a tiny TSH around 0.004-0.009.
The optimal metabolic rate should give you a stable 36.6 under the tongue on waking and 37.0 by dinner. Personally, I recommend patients to measure sublingual temperature every morning and record somewhere on the phone in order to understand what happens to T3 cell levels and free cortisol levels in general.
Causes of hypothyroidism
According to the first and second parts of the best for hypothyroidism book "Stop the thyroid madness", the main causes of hypothyroidism are: unbalanced nutrition \ malabsorption (poor absorption), inflammation, toxicity, removal of thyroid, estrogen dominance, hypophysis \ hypothalamus dysfunction.
Malabsorption / Unbalanced Nutrition
For proper production of thyroid hormones, their conversion, transport and utilization by the cell in the body, there should be a wealth of a number of trace elements + free (!) Cortisol, and there should also be no hidden inflammation. If a person receives less / underestimates some of the microelements that are critical for the thyroid gland, he will eventually develop hypothyroidism, even if the thyroid gland itself is completely functional. The most frequent are deficiencies of iodine, iron, zinc and selenium, but there may be B12, vitamin D, magnesium, other B vitamins, etc. Common causes of malabsorption (poor absorption / absorption) are hydrochloric acid deficiency, dysbacteriosis, enzymatic deficiency and a long list of other causes. Given that iron deficiencies (more than 30% of the world's population) according to WHO, iodine and zinc are among the top most common deficiencies, there is nothing surprising in such a wild number of hypothyroidism in society. More on this in the sections "The Importance of the Sufficiency of Micronutrients" and "Hydrochloric Acid Deficiency."
Hidden inflammation
Normally, inflammation is a healthy and positive reaction of the immune system to the presence of infection, virus, bacteria or fungus, as well as cell damage in the event of burns, wounds, injuries and so on. But if it develops into a chronic one, it becomes the worst enemy of the thyroid gland. For some patients, inflammation may be obvious, but not for most.
Elevated levels of inflammation inhibit the activity of all endocrine organs, including the thyroid gland. Inflammation leads to an increase in inverse m3, a decrease in the function of the thyroid receptor of the cell, thereby creating resistance. With inflammation, you do not cure hypothyroidism, no matter how many hormones you take.

C-reactive protein, erythrocyte sedimentation rate (ESR) and ferritin can help you diagnose inflammation (above 200 may be inflammation).
Autoimmune thyroiditis, a disease in which the immune system begins to attack its own thyroid gland and eventually destroys it, is one of the causes of inflammation and one of the most common causes of hypothyroidism.
For more information about the causes and methods of eliminating inflammation in the section hidden inflammation.
Toxicity
Unfortunately, modern human habitat is replete with toxic halogens, heavy metals and xenoestrogens, which damage a number of organs and systems in the body, as well as suppress the thyroid gland.
Toxic bromine, fluorine and chlorine belong to the same halogen family as iodine. This means that they compete with each other for cell receptors on the basis of competitive inhibition and most often wins it with bromine. Their entry into the body not only leads to iodine deficiency, but also undermines the chemical reactions in which iodine is involved. More on this in the "Iodine" section.
Such heavy metals as lead, mercury, arsenic, cadmium and aluminum damage the work of enzymes and lead to hypothyroidism.
Xenoestrogens such as bisphenol-a, phthalate, pesticides, herbicides, petroleum products, and soy are synthetic analogues of estrogens. Their excess causes hormonal imbalance (estrogen domination), in response to which the body binds almost all cortisol, which leads to adrenal insufficiency and hypothyroidism.
Surgical removal of the thyroid gland or its killing with radioactive iodine
Lazy non-developing doctors do not like to go deep into the causes of Baseedov-Graves autoimmune disease and cure it with a low-dose diet or naltrexone (as experts in the west do), but they love to remove it. After that, the patient is put on T4 monotherapy (the worst replacement therapy ever invented by man) and his life slowly turns into hell. There are a lot of examples of such a scenario. Of course, autoimmune diseases do not disappear anywhere, because their cause (usually leaky bowel syndrome) remains intact.
Postpartum hypothyroidism. Estrogen dominance
Many patients report that they have received hypothyroidism or autoimmune thyroiditis after the birth of a child. One reason is postpartum estrogen dominance. The levels of estrogen (estradiol + estrone) and progesterone should be in a certain proportion / balance, and after giving birth, women experience a drop in the levels of both. But in some, progesterone drops more significantly than estrogen and this leads to estrogen dominance (or a deficiency of progesterone in a different way). Estrogen domination disrupts the arches of the ovaries-thyroid-adrenal glands and leads to serious hormonal problems. However, there may be other causes of postpartum hypothyroidism.
Tumor / damage to the pituitary or hypothalamus
Since these glands play a key role in regulating the functioning of the thyroid gland, a drop in their functionality leads to problems with other glands.
Hemochromatosis
In hemochromatosis (iron overload), the body rebuilds hormones, linking almost all cortisol and aldosterone (adrenal insufficiency), which, of course, automatically leads to hypothyroidism, regardless of the state of the thyroid gland.
Autoimmune thyroiditis
One of the common causes of hypothyroidism is autoimmune thyroiditis (Hashimoto's thyroiditis, Hashimoto syndrome, AIT), first described in 1912 by the Japanese specialist Hakaru Hashimoto. In autoimmune diseases, the immune system attacks various organs and tissues of its own, and in the case of AIT, the thyroid gland is the target. Regular attack by antibodies over time leads to damage and loss of functionality of the thyroid, development of nodes and goiter, and in some cases to the complete destruction of the gland.
How is it diagnosed?
You need to pass two (!!) antibody tests:
- antibodies to thyroglobulin (TG)
- antibodies to thyroperoxidase (TPO)
Thyroglobulin is a protein containing the amino acid Tyrosine, which is a precursor of the thyroid hormone thyroxine (T4). The process of attaching iodine to tyrosine is called "iodization" and is carried out by the enzyme thyroperoxidase (TPO).
What causes immunity to attack its own organs and tissues?
If you ask Russian doctors, most of you will answer that the cause is unknown and the disease is not treated. But, fortunately, the reasons are unknown only to lazy and non-developing doctors, who do not read modern studies and books.
Causes of AIT:
1) Selenium deficiency. In the body there are a number of proteins dependent on selenium. The most important of these are deiodine enzymes (convert t4 to t3 or reverse t3), as well as glutathione peroxidase, which protects the cells of the thyroid gland from damage by hydrogen peroxide. With selenium deficiency, glutathione peroxidase cannot effectively protect the thyroid cells from destruction by hydrogen peroxide, which, according to the theory, being damaged, are recognized by the immune system as foreign and are attacked. In a number of studies in different countries, the use of selenium in a dose of 200-400 mcg / day either significantly reduced antibodies, or even antibodies completely normalized. More often the study shows the reduction of antibodies to TPO.
2) Iodine deficiency. Some patients report that the use of iodine (necessarily with nutrient companions like selenium) reduced their antibodies. It is always important to remember that taking iodine against a background of selenium deficiency can be toxic. On the heads of most endocrinologists, the myth is still walking that taking iodine can aggravate AIT and lead to the growth of antibodies. This hypothesis was based on two observations: 1) a study on mice with diabetes without obesity (NOD mice), where iodized drinking water provoked AIT 2) observation that salt iodization programs coincided with an increase in the number of AITs. Subsequently, in a number of studies, the relationship between iodine intake and antibody growth has been refuted, but this information has not yet reached many. And despite salt iodization programs, iodine intake has decreased by 50% over the past 40 years. Among patients with AIT, the absolute majority (93%) have iodine deficiency as observed by David Brownstein, one of the leading experts on iodine on the planet.
3) Leaky bowel syndrome + molecular mimicry. Vitamin D deficiency. Normally, intestinal permeability allows small molecules of amino acids, glucose, vitamins, minerals and other useful nutrients to flow into the bloodstream and to retain large "harmful" molecules - undigested food, toxins, bacteria, viruses, fungi, etc. As a result of an irregular diet (usually due to gluten or lactose, but maybe because of other products), or bacterial imbalance, or chronic stress, or low cortisol - pores in the intestinal walls increase, permeability takes off, the intestines are inflamed and now toxins , bacteria, undigested gluten and viruses - get into the sterile environment of the bloodstream. The immune system sees in the bloodstream everything that should not be there, regards them as potentially harmful substances and directs its forces to eliminate! In order to distinguish between "our own" and "alien" ones, the immune system uses a sequence of amino acids, and unfortunately for us, some undigested proteins (like gluten, for example) or bacteria (Yersinia) have an amino acid sequence that is similar to the tissues of the thyroid gland. Thus, due to the molecular similarity with some proteins in the bloodstream, various organs and tissues fall under the attack of immunity. This condition is called leaky bowel syndrome or increased intestinal permeability syndrome. This theory has many supporters and it explains well why a gluten-free diet reduces the level of antibodies in people with AIT. Vitamin D deficiency is one of the predisposing factors for the development of leaky bowel syndrome.
4) Insufficiency of hydrochloric acid in the stomach. Normally, hydrochloric acid effectively breaks down proteins into amino acids, which are subsequently recognized by the immune system as food / building material. With a deficit of hydrochloric acid, proteins turn out to be "underdeveloped" and, accordingly, unidentified by the immune system, which subsequently begins to produce antibodies to these proteins. The lack of hydrochloric acid paves the way for autoimmune diseases.
Treatment
- Treat hypothyroidism. A big step is treatment with natural thyroids, not synthetic T4. When switching to nat. Thyroid gland initially antibodies can grow, but as their dose increases and hypothyroidism is eliminated, antibodies decrease and this is probably due to the improved performance of the immune system.
- 100% gluten free diet
- Selenium 200-400 mcg / day
- Iodine by download protocol
- Eliminate the deficiency of hydrochloric acid
- Naltrexone in low doses helps many to significantly reduce the level of antibodies.
Hidden inflammation
Normally, inflammation is a healthy and positive reaction of the immune system to the presence of infection, virus, bacteria or fungus, as well as cell damage in the event of burns, wounds, injuries and so on. But if it develops into a chronic one, it becomes the worst enemy of the thyroid gland. For some patients, inflammation may be obvious, but not for most.
Elevated levels of inflammation inhibit the activity of all endocrine organs, including the thyroid gland. Inflammation leads to an increase in inverse m3, a decrease in the function of the thyroid receptor of the cell, thereby creating resistance. With inflammation, you do not cure hypothyroidism, no matter how many hormones you take.
C-reactive protein, erythrocyte sedimentation rate (ESR) and ferritin can help you diagnose inflammation (above 200 may be inflammation). An elevated c-reactive protein or ESR automatically means inflammation. Excessive ferritin 200+ probably means inflammation, but there may be other causes. More details in the section "Iron".
The most common causes of inflammation:
- Pro-inflammatory food. Hidden food allergies and sensitivities. The main candidates are gluten, milk, eggs, soy, yeast, corn, peanuts, nuts, and in rare cases, nightshade (potatoes, tomatoes, bell pepper, eggplant). In patients with AIT, inflammation most often creates gluten.
- Hidden infections in the intestines (such as helicobacter pylori, for example). Dysbacteriosis, problems with absorption, problems with pancreatic enzymes, candidiasis, parasites, latent viral infection.
Other reasons:
- hormonal imbalances
- autoimmune thyroiditis
- chronic stress
- low free cortisol
- non-alcoholic fatty liver disease
- heavy metal toxicity
- excess consumption of foods high in oxalate
- dysglycemia - instability of blood sugar levels
- Helicobacter pylori bacterium
- cancer
How to remove inflammation?
1) You should try to find its cause, although it is not easy. If specialized testing for intolerance / sensitivity to various products (food sensitivity test) is available to you, you must do them. If not, then I would advise you to remove all gluten from the diet (wheat, rye, barley, oatmeal), all milk (including cheese, yogurt, ice cream, probiotics with milk, etc.), eggs, soy, yeast, corn, peanuts, nuts, and nightshade, and then observe changes in inflammatory markers a month later. Regardless of whether they cause you inflammation or not, gluten, milk, soy, yeast, corn are junk toxic products that ruin your health. Good western doctors do not allow members of their families to consume these products.
There are 3 types of rejection by the body of a specific product: 1) intolerance (intolerance) is a purely mechanical problem, due to the absence or underproduction of enzymes that break down proteins / carbohydrates in this product. For example, underproduction of the lactase enzyme leads to the fact that the milk carbohydrate lactose cannot be adequately digested, the patient gets diarrhea or bloating. This type of intolerance does not involve immunity. 2) Allergy - an instantaneous immune reaction to the product, which can occur within a few minutes or even seconds after use. Runny nose, urticaria, sneezing, pain in the eyes, bronchospasm, asthma attacks. Allergies are dangerous to health, but they are much easier to detect experimentally. 3) food sensitivity (food sensitivity) is a delayed immune response that can last for weeks and months, giving chronic inflammation if the patient regularly uses the product. No urticaria, nausea or asthma attacks. This product slowly and secretly disfigures your health, giving you symptoms that are extremely difficult to link to food: chronic fatigue, weakened immunity, hypothyroidism, etc. The second and third types are united by what the immune system considers this product to be a threat to health activates his strength to fight him. And, as a rule, such a reaction is found on new “civilization” products that our distant ancestors did not use 20 thousand years ago: gluten, jelly, corn, eggs, soybeans, etc.
2) Get your intestines clean. Testing for helicobacter pylori (blood is not informative) and other bacteria, testing for the presence of gastritis, candida, restoration of intestinal microflora, etc.
Remove refined sugars, because they aggravate insulin resistance, weight gain and inflammation, as well as provoke the growth of Candida fungus.
Minimize the intake of high oxalate foods.
3) Try to cure hypothyroidism and adrenal insufficiency. Cortisol itself is a strong anti-inflammatory hormone. Fully cure for inflammation will not succeed, but it will be possible to significantly improve the condition.
4) Optimize levels of vitamin D, which is a natural anti-inflammatory agent.
5) Exercise can significantly reduce the level of inflammation. But do not bend if you have lowered free cortisol.
6) Increase the intake of anti-inflammatory omega-3 fats (fish oil) and minimize the consumption of pro-inflammatory omega-6 fats (peanuts, sunflower oil, corn, peanut, saffrole and soy)
7) Naltrexone in low doses significantly enhances \ normalizes the immune system and in some cases helps reduce inflammation. Extremely cheap and safe.
8) There are a number of supplements that are known for their anti-inflammatory properties. Below I will list the main ones. But the problem of such additives, as well as naltrexone and points 4, 5, 6 is that they do not eliminate the cause of inflammation, but only struggle with its consequences. For example, naltrexone enhances immunity by increasing the production of endorphins, and anti-inflammatory supplements only block various inflammatory agents. Of course, if the cause of your inflammation in a regularly consumed product, nothing but the complete exclusion of it from the diet will not help you.
Additives: turmeric, selenium, bioflavonates, ginger, basil, vitamin C, vitamin K, vitamin D and others.